How Particulate Matter injures airways and promotes exacerbation of pulmonary diseases
An international study led by the University of Bern has investigated the effects of ambient Particulate Matter (PM) from human and natural sources on human lung cells. Thereby, the researchers found damage to the cellular defense system of the lungs, which furthers the aggravation of pre-existing lung diseases like asthma or Cystic Fibrosis. Man-made PM components, among them from wood-burning fires and road traffic are mainly responsible for the investigated health damaging effects.
Air pollution, in particular through particulate matter, belongs beside high blood pressure, smoking, diabetes, and overweight to the leading five health risks worldwide. Children, pregnant women, the elderly and persons with cardiovascular or pulmonary diseases are especially vulnerable. According to the Swiss Federal Office for the Environment, every year more than 2000 people die prematurely from the consequences of air pollution in Switzerland and 4.2 million worldwide.
There is only limited information about which particle characteristics are responsible for the observed adverse effects and which biological pathways in airway cells are affected. The international research team under the leadership of the lung researcher Marianne Geiser from the Institute of Anatomy at the University of Bern and the aerosol researcher Josef Dommen from the Paul Scherrer Institute (PSI) demonstrate for the first time the direct link of cell damage by PM and inflammatory processes.
One of the main innate defense systems of the lungs is weakened, furthering the aggravation of pre-existing lung diseases. In addition, the researcher found that the investigated health-damaging effects are mainly due to PM components from human sources. The study is published today in the Scientific Journal «PLOS ONE».
Particulate matter and health effects
The causal link between PM inhalation and adverse health effects has been scientifically proven for a long time. In healthy people, the well-developed defense mechanisms in the lungs normally render deposited particles ineffective and remove them from the lungs as quickly as possible. However, if inhaled particles manage to overcome these defense mechanisms due to their physico-chemical properties, there is a risk for irreparable damage to the lung tissue.
Persons with asthma, chronic obstructive pulmonary disease (COPD) or Cystic Fibrosis (CF) are particularly vulnerable. The present study investigated, which particle characteristics are responsible for which damage to the airway cells, which effect PM has on the cellular defense mechanisms, and finally, which changes in the defense system affect disease progression.
Realistic experiments
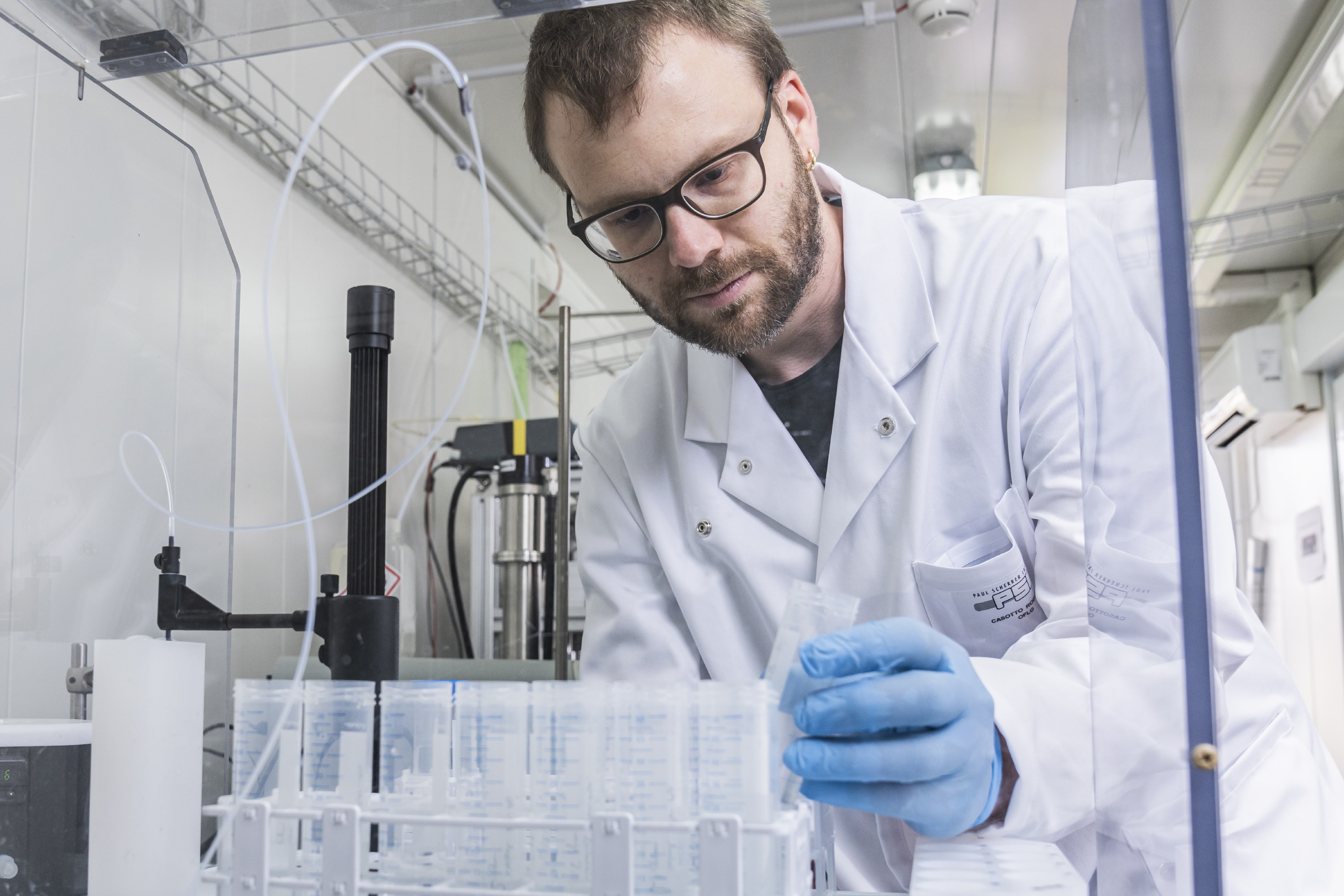
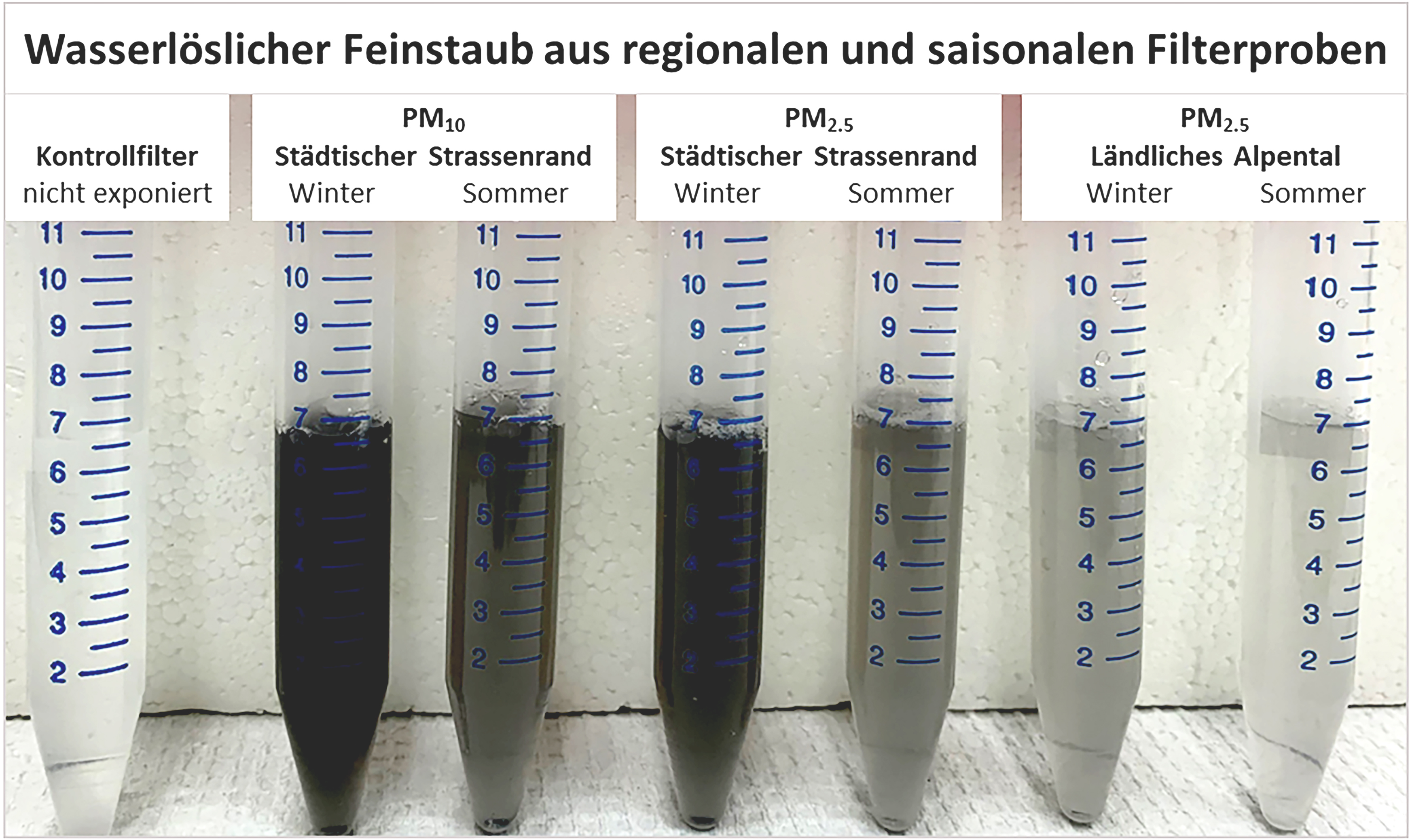
For the investigation, water-soluble PM with different physical and chemical properties from regional and seasonal filter probes were extracted, and the so-called oxidative potential (OP) of extracted particles was determined. The OP is a measure for the capacity of PM to degrade antioxidants, which can lead to cell and tissue damage. Thereafter, the airway cells were exposed to different particle doses. “For the experiments, we used realistic cell models of the inner airway surface”, explains Marianne Geiser. “This allows the deposition of potentially toxic particles on cell cultures of healthy and diseased airways, to assess their hazard potential for particularly vulnerable persons, who could not participate in a study because of ethical reasons”.
This was made possible by an in-vitro model system for realistic inhalation toxicology, which was developed by Marianne Geiser in collaboration with Swiss and american partner institutions. The results showed concomitant increases of cytotoxicity and pro-inflammatory mediators in healthy as well as in Cystic Fibrosis airway cells. “This indicates a link between cytotoxicity by PM and inflammatory processes”, says Zaira Leni, first author of the study.
Thereby, an imbalance in one of the most important innate defense systems in lungs, the antioxidant defense, was caused. While the innate defense system in healthy cells could prevent the progression of the inflammatory response, it could not be intercepted by the compromised airway cells. This resulted in enhanced cell death and, thus, promotes disease exacerbation. Moreover: “These responses also reduce the ability of airway cells to react appropriately to a subsequent viral or bacterial infection,” explains Marianne Geiser.
Fine dust from human sources are the most harmful
In a partner study led by the Paul Scherrer Institute, which is published today in the Scientific Journal “Nature”, the components and source apportionments of ambient PM were evaluated and allocated to the different emission sources by means of statistical procedures. The researchers found that the OP comes mainly from wood-burning fires and metal emissions from brake and tire wear from road traffic.
“In a parallel cell experiment, we could show for the first time that the OP correlates well with the observed inflammatory responses”, says Kaspar Daellenbach from PSI. The exposure of the European population to PM, evaluated by means of air quality models, showed that the mass and the OP of PM in the different regions is not determined by the same emission sources. It is therefore suggested that the reduction of PM mass is not sufficient, but that emission sources with high OP need to be reduced.
”The state-of-the-art measurement methods used in our study, the interdisciplinary approach, and the resulting outcomes all constitute a further important step in the research on air pollutants and the health-damaging mechanisms”, says Josef Dommen from PSI. The researchers are convinced that the inclusion of health-relevant PM components in regulatory guidelines would lead to health improvement and protection of the vulnerable population.
The study was supported by the Swiss National Science Foundation (SNSF).
Publication details:Z. Leni, L.-E. Cassagnes, K.R. Daellenbach, I. El Haddad, A. Vlachou, G. Uzu, A.S.H. Prévôt, J.-L. Jaffrezo, N. Baumlin, M. Salathe, U. Baltensperger, J. Dommen, M. Geiser. Oxidative stress-induced inflammation in susceptible airways by anthropogenic aerosol. PLOS ONE, 18. November, 2020; https://doi.org/10.1371/journal.pone.0233425. |
2020/11/18