Precision oncology helps prostate cancer patients
Researchers at the University of Bern and University Hospital Bern have achieved a breakthrough in a particularly aggressive form of prostate cancer. In tissue samples from advanced brain metastases, they were able to establish the genetic profile of the cancer cells. These findings show for the first time that affected patients could benefit from target treatment, from which they have so far not been eligible.
Around 6,600 men are diagnosed with prostate cancer in Switzerland every year. It is the second most common cause of cancer-related death in men after lung cancer. Dangerous are advanced stages in which cancer cells have spread to other organs and form so-called metastases. However, unlike other cancers such as breast or lung cancer, the extremely dangerous metastases in the brain are very rare in prostate cancer. Only 1.5 percent of advanced cases have been diagnosed as brain metastatic prostate cancer (PCBM), according to a 2020 review study. As a result, PCBM cases have been poorly studied.
Researchers led by Mark A. Rubin of the University of Bern and University Hospital Bern have now filled this gap with the first major study of prostate cancer brain metastases. In their study, they described the molecular biological profile of PCBM cells. According to the study, these cells have clustered alterations in the cellular repair mechanism, which in healthy cells repairs everyday damage in the genetic strand. "The changes resemble the genetic signature of other cancers for which effective drugs are available", says Mark A. Rubin, director of the Department for BioMedical Research and president of the Bern Center for Precision Medicine at the University of Bern and University Hospital of Bern. "This is positive news. Because it means there's nothing standing in the way of targeted treatment for at least some of patients with PCMB". The study was published online in the journal Nature Communications.
Alterations in the repair mechanism of cancer cells
In cancer cells, the cells' repair mechanisms are altered in such a way that they can no longer patch up certain damage in the genetic strand and therefore proliferate uncontrollably. In metastatic cells, an alternative repair mechanism steps into the breach, allowing the cancer cells to thrive. However, drugs known as PARP inhibitors specifically block this alternative repair mechanism and lead to the death of the cancer cells. However, these only work if the changes in the dangerous cells show a certain pattern in the primary repair mechanism.
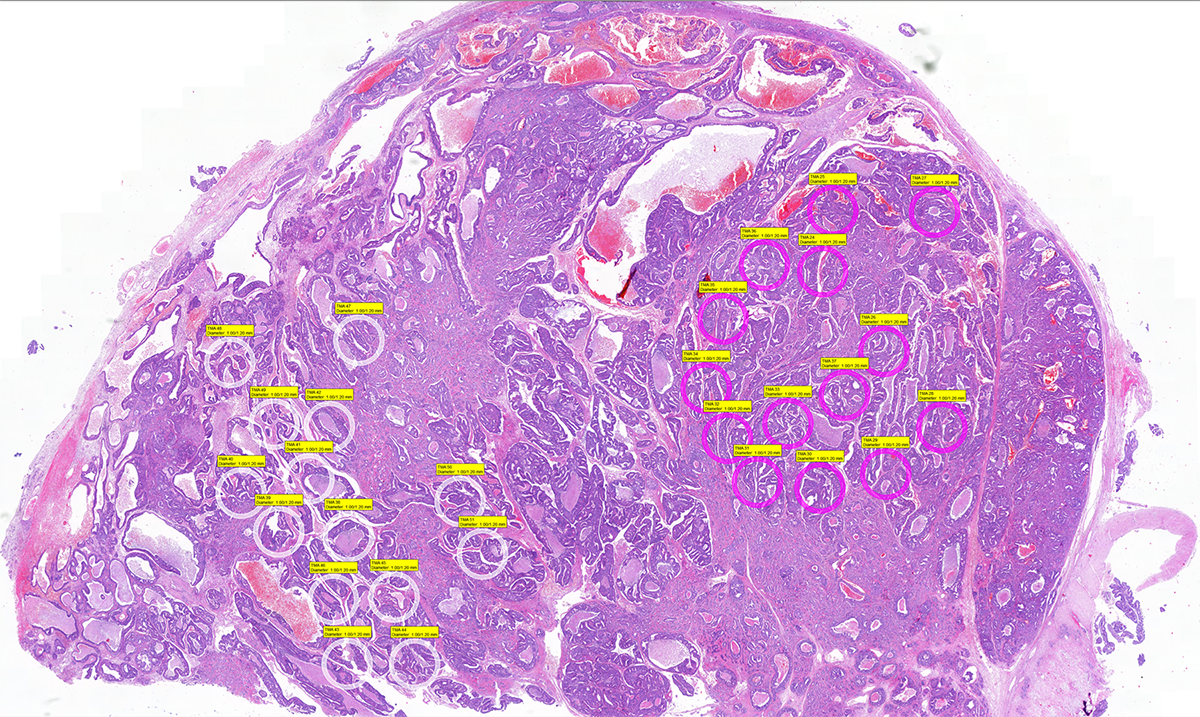
In their study, the researchers examined prostate cancer brain metastases from 51 PCMB patients obtained from hospitals throughout Switzerland and from a partner institution in the USA. The analysis showed that alterations in the primary DNA repair mechanism were detected in all tested samples with brain-metastasizing prostate cancer cells. In about 20 percent of the patients studied, the researchers detected the exact genetic pattern in which, according to a study published in 2020, administration of PARP inhibitors significantly increased survival rates in those affected. "One in five patients with brain metastatic prostate cancer could therefore benefit from therapy with these targeted drugs", says Mark A. Rubin.
Prime example of precision oncology
At the same time, genomic analysis of brain metastases and comparison with other cancers opens new doors for basic research. "If we understand why there are fewer brain metastases in prostate cancer compared to other tumor types, we can learn in the future what changes in the cells make them malignant", explains Mark A. Rubin.
The work is also seen as a prime example of precision oncology in which treatment concepts are increasingly tailored to the specific patient. According to this approach, information on genetic profile of tumor cells of each individual patient is used to design a treatment using drugs that would target the specific alterations observed.
The study was supported, among others, by the Swiss Personalized Health Network (SPHN), the Swiss Cancer League, and in part by the Prostate Cancer Foundation, the U.S. National Institutes of Health (NIH), and the Prof. Dr. Max Cloëtta Foundation.
Publication:Antonio Rodriguez-Calero, John Gallon, Dilara Akhoundova, Sina Maletti, Alison Ferguson, Joanna Cyrta, Ursula Amstutz, Andrea Garofoli, Viola Paradiso, Scott A. Tomlins, Ekkehard Hewer, Vera Genitsch, Achim Fleischmann, Erik Vassella, Elisabeth J. Rushing, Rainer Grobholz, Ingeborg Fischer, Wolfram Jochum, Gieri Cathomas, Adeboye O. Osunkoya, Lukas Bubendorf, Holger Moch, George Thalmann, Charlotte K. Y. Ng, Silke Gillessen, Salvatore Piscuoglio & Mark A. Rubin. Alterations in homologous recombination repair genes in prostate cancer brain metastases. Nat Commun, 3 May 2022, https://www.nature.com/articles/s41467-022-30003-5 |
Bern Center for Precision Medicine (BCPM)The Bern Center for Precision Medicine (BCPM) was founded in 2019 on the initiative and with the support of the Canton, the University of Bern and Inselspital, Bern University Hospital. The BCPM is active in research, networking and training. The center is dedicated to promoting approaches in precision medicine by supporting research and development of medical diagnoses and therapeutic methods. It offers an interdisciplinary network for researchers and clinicians from various fields and faculties and unites more than 70 members. Through graduate schools, the BCPM will also provide the best possible education for the next generation of care takers and researchers. As a result, it is securing the long-term benefits that precision medicine brings to healthcare. |
Department for BioMedical Research (DBMR)The Department for BioMedical Research (DBMR) of the Faculty of Medicine at the University of Bern, led by Prof. Dr. med. Mark A. Rubin, was established in 1994 by the University of Bern and Inselspital, Bern University Hospital. The DBMR is comprised of 13 research programs with approximately 100 participating individual labs and several independent research labs whose research spans across all biomedical fields. In order to bridge the gap between bench and bedside, the DBMR promotes an integrative perspective to clinical research with a strong emphasis in the development of translational approaches, the use of omics and other cutting-edge technologies, as well as extensive interaction and collaboration between laboratory-based and patient-oriented clinical research. The DBMR is also committed to fostering the careers of young academics. |
2022/05/11