Significant vulnerability in prostate cancer detected
Researchers at the University of Bern led an international team that has identified a novel vulnerability in advanced prostate cancer that is no longer responding to hormonal therapy. These findings could lead to the development of new treatment approaches for men suffering from the most aggressive form of prostate cancer.
Prostate cancer is the third predicted cause of cancer deaths in EU men with 78,800 deaths in 2020 and a death rate of 10 per 100 000 population. While localized prostate cancer is most often effectively treated through surgery and radiotherapy, the mainstay of treatment for metastatic prostate cancer are anti-androgen (hormonal) therapies; however, resistance to these therapies ultimately develops.
To date, most studies on treatment-refractory cancers have focused on changes in the DNA sequence in cancer cells – genetic mutations – as a mechanism of therapy resistance. However, cancers can also become treatment-resistant through radical shifts in cell identity, yielding relapses that may bear little resemblance to early-stage pre-treatment tumors. This phenomenon, known as lineage plasticity, is a less understood mechanism of tumor progression. Similar to camouflage, this plasticity allows cancer cells to change appearance and growth machinery to evade therapy. This transformation is observed in a number of treated cancers, including prostate and lung cancer. In prostate cancer, a switch to a highly aggressive form of the disease is seen in about 10-15% of men treated with hormone therapy and to date, there is no standard-of-care treatment for these men.
Identity switch in cancers usually occurs in the setting of specific genomic mutations, but studies previously published by Dr. Rubin’s group at the University of Bern and Inselspital, University Hospital Bern showed that these events are not sufficient to enable such transformation. If changes in the DNA are not sufficient, what other changes that occur in cancer cells could enable this transformation? Dr. Rubin’s team study focused on "epigenetic" changes. These changes do not involve alterations of the DNA genetic code but often regulate gene activity and expression. One type of epigenetic regulators are multi-protein complexes which, depending on their composition, influence the way a cell uses the information contained in its DNA. This, in turn, determines cell identity. "Cancer cells can hijack this machinery to favor their growth over the surrounding normal cells", explains Rubin.
A novel dependency of prostate cancer cells identified
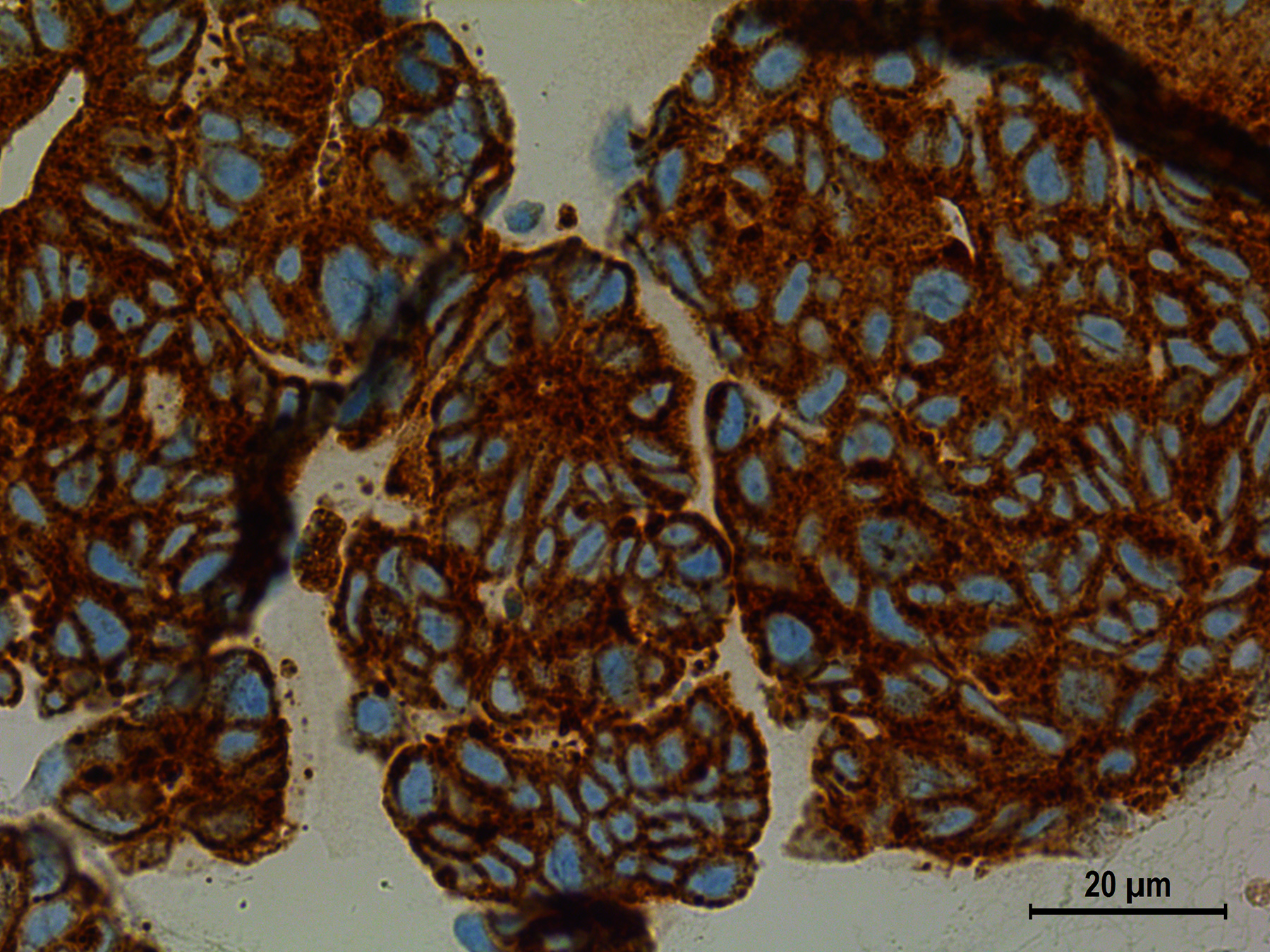
Post-Doctoral Researchers in the Rubin laboratory, Dr. Anke Augspach (Post-doctoral fellow, University of Bern) and Dr. Joanna Cyrta (formally Weill Cornell Medicine, currently at Institut Curie, France), have nominated dependency on an important epigenetic regulator, called the SWI/SNF complex, for prostate cancer cells to grow. "This dependency can be explored as a vulnerability to developing new treatment approaches for advanced prostate cancers resistant to hormone treatment", says Anke Augspach. The SWI/SNF complex remodels a cell’s DNA to determine which part of the information is accessible for the cell to use, and which part remains silent. Such regulation can have a multifold effect on cells, for example on growth or differentiation.
Dr. Rubin’s team showed that specific components of the SWI/SNF complex are highly expressed in the most aggressive prostate cancers – the ones that have undergone an "identity switch". "As the SWI/SNF complex is composed of up to 15 different proteins, this was a technically challenging study", says Rubin. By focusing on several key members of the complex, Dr. Rubin’s team observed that several prostate cancer cell lines are dependent on the SWI/SNF complex for their growth. The findings have been published today in Nature Communications. Future work by this team will continue to explore the mechanisms by which SWI/SNF may be involved in the process of prostate cancer cell plasticity. The development of novel drugs to help patients where there is no standard of care options left is a major focus of the Bern Center for Precision Medicine (BCPM) – a joint initiative of the University of Bern and the Insel Gruppe.
This project has received funding from the NIH/NCI WCM and MSKCC SPOREs in Prostate Cancer, the European Research Council (ERC) and the Swiss National Science Foundation. The University of Bern and Cornell University have filed a patent application on SWI/SNF regulation in the fields of advanced prostate cancer as biomarkers and for therapy. Joanna Cyrta, Anke Augspach, and Mark Rubin are listed a co-inventors.
Publication details:Cyrta J, Augspach A, de Filippo MR, Prandi D, Thienger P, Benelli M, Cooley V, Bareja R, Wilkes D, Chae S-S, Cavaliere P, Dephoure N, Uldry A-C, Lagache SB, Roma L, Cohen S, Jaquet M, Brandt LP, Alshalalfa M, Sboner A, Feng F, Wang S, Beltran H, Lotan T, Spahn M, Kruithof-de Julio M, Chen Y, Ballman KV, Demichelis F, Piscuoglio S, Rubin MA. Role of Specialized Composition of SWI/SNF Complexes in Prostate Cancer Lineage Plasticity. Nat Commun. 3 November 2020, https://www.nature.com/articles/s41467-020-19328-1 |
Bern Center for Precision Medicine (BCPM)The Bern Center for Precision Medicine (BCPM) was founded in 2019 on the initiative and with the support of the Canton, the University of Bern and Inselspital, Bern University Hospital. The BCPM is active in research, networking and training. The center is dedicated to promoting approaches in precision medicine by supporting research and development of medical diagnoses and therapeutic methods. It offers an interdisciplinary network for researchers and clinicians from various fields and faculties and unites more than 70 members. Through graduate schools, the BCPM will also provide the best possible education for the next generation of care takers and researchers. As a result, it is securing the long-term benefits that precision medicine brings to healthcare. |
2020/11/03